Medicare Behavioral Health Conflict of Interest Reporting and Review
Direction of High-Need, High-Price Patients: A Realist and Systematic Review
Research Protocol December iv, 2019

I. Groundwork and Objectives for the Review
Groundwork
Payers in the U.Southward. health care system, specially Medicare and Medicaid, are increasingly requiring health care systems, coordinated care organizations, and health care professionals to progress from payment through fee-for-service arrangements toward alternative payment models that include financial adventure.1-4 For this reason, the claiming of addressing high-demand, high-cost (HNHC) patients is increasingly pressing. Health intendance systems participating in alternative payment models, particularly those that include financial risk, acknowledge that their success in these models depends, in large part, on their effectiveness in addressing the intendance and costs for HNHC patients.5,6
Although HNHC patients represent a small proportion of the patient population, they business relationship for a substantial proportion of health care costs.vii-11 Health intendance systems would like to accomplish two goals in relation to HNHC patients: (1) reduce their health care use that is potentially preventable or modifiable, which is oft astute care in the emergency department (ED) or infirmary inpatient setting,12-sixteen and (ii) increase their quality of intendance.xiv-sixteen Despite strong motivation to address the burden of HNHC patients, multiple challenges and controversies complicate approaches to identifying HNHC patients and determining the causal mechanisms of complex interventions that affect health care utilization, cost, and quality of care.
Purpose of the Review and Approach
This review has 3 main objectives, all with the shared purpose of identifying actionable bear witness to support informed decisions for clinicians, health care systems, and payers. The first is to describe approaches to identifying HNHC populations. The second is to develop and refine theory explaining why item interventions, in various circumstances, are more likely to be successful in irresolute potentially preventable or modifiable health intendance use and improving quality of intendance for HNHC patients. The 3rd is to review the testify supporting the overall effectiveness of these interventions. We will use qualitative and quantitative synthesis methods in conducting the review.
Defining High-Need, High-Price Patients
Researchers and practitioners accept non decided on a single definition of HNHC patients, those loftier-need patients for whom high costs are potentially preventable or modifiable. One direct approach is to identify the patients with the highest costs during a historical time period, but no consensus has been reached on the appropriate duration of the time menses and the number and types of utilization.12,13 Also, focusing on toll lone can obscure detecting high-demand patients. A large per centum of high-cost patients utilize this level of intendance for a relatively brusque period of time, and it is the appropriate option for treating their condition (eastward.thou., certain types of cancer or orthopedic surgery patients).17 A second approach is to place HNHC patients based on diagnoses, such as individuals with multiple co-occurring chronic conditions (one or more of which may be a behavioral health condition).eighteen,19 Relying chiefly on a diagnostic definition, nonetheless, ignores that not all high-need patients are HNHC. A large percentage of high-need patients use care accordingly, even if it may be costly (i.due east., needed health care is received through ongoing relationships with primary care and specialist providers). Further refinement in defining and predicting whether individuals with high-need chronic conditions are at gamble of being loftier users of potentially preventable or modifiable health care may be related to identifying additional risk factors.xx Overall, HNHC patients include those patients for whom reducing use of loftier-cost health intendance services in favor of other types of intendance is theorized to consequence in better intendance and ameliorate outcomes.
To facilitate our synthesis of the evidence on approaches to identifying and describing HNHC patients and to explore the relationships among the approaches, nosotros will conduct a "best fit" framework synthesis.21 Consistent with this arroyo, nosotros begin from an a priori identified framework that we will use to sort evidence into themes across included studies (i.e., the distinguishing characteristics and reasons why some patients are HNHC). During our review of the evidence, nosotros will apply an iterative process to consider new themes that are not captured in the initial framework. In the terminate, we will nowadays a summary of the data and syntheses of the prove and our conclusions inside a framework corresponding to our final conceptual model.
We propose to begin the synthesis using the taxonomy developed by the National University of Medicine in their report Constructive Care for High-Demand Patients: Opportunities for Improving Outcomes, Value, and Health as our a priori framework.20 This taxonomy groups HNHC patients first based on their clinical and functional characteristics. Amid the half-dozen patient groups presented in the taxonomy, 4 run into the inclusion criteria for this review: nonelderly disabled, multiple chronic weather condition, major complex chronic condition, and delicate elderly. (the boosted 2 categories, children with circuitous needs are advancing illness/cease-of-life care are outside the scope of the review.) Within these assigned groups, the taxonomy proposes additional, cantankerous-patient group cess based on behavioral health factors and social chance factors that are believed to influence how individuals use health care and increment the risk of receiving fragmented care. Behavioral health factors include persistent and serious mental illness, substance abuse, cerebral decline, and chronic toxic stress. Social hazard factors include depression socioeconomic status, low health literacy, social isolation, community deprivation, and housing insecurity.
Agreement Interventions for Loftier-Need, High-Toll Patients
To gain a greater understanding of the complex alternative payment and delivery models, social interventions, and health programs that are used to address wellness intendance utilization among HNHC patients, we will use a realist review approach. Consistent with this approach, our goal is to explain what works (or fails), for whom, under what circumstances, and why.22 We will seek to identify, elucidate, and refine the various underlying theories that could explicate the approach of dissimilar complex interventions, explore implementation bondage, appraise intermediate outcomes, and examine modifications or adaptations applied in various circumstances.22
Using the terminology of the realist arroyo, reviewers seek to decide how particular contexts have "triggered" mechanisms to generate outcomes.23 The relationships are summarized as context + mechanism = outcome (CMO). Context is the "backdrop," the variety of features that can bear upon the implementation of a programme, including participant characteristics, programme setting, resources, and history that trigger or alter the processes through which an intervention produces an upshot.24 Mechanisms are the underlying processes that piece of work in specific contexts to generate the outcomes of interest. The intervention is thought of as manipulating or changing the context and so that specific mechanisms tin can exist triggered.24 Finally, the upshot is the impact or behaviors that arise from the inter-relationship between mechanisms and contexts.
Using a systematic review approach, 1 would draw a group of studies of interventions as customs health workers whose chore is to increase the percentage of patients who regularly get to master care medico office visits. Using a realist approach, i would seek to describe why the customs health worker intervention might work. For example, when isolated patients living in a large city, who must be self-reliant in getting to their doctors' appointments are provided with one-on-1 aid from a community health worker on how to utilize the coach organization (C), the patients are more likely to get to their office visits (O) considering they are more confident and take greater agency that they will exist successful (M). A second CMO configuration in the causal pathway might be that regular visits with a clinician (C) result in greater medication adherence and fewer visits to the ER (O) considering patients trust that their clinicians know them and care about their welfare (1000).
In addition, to further back up the goal of producing actionable information, we will also use traditional Evidence-based Practice Center systematic review methods to synthesize the evidence of the overall effectiveness of the interventions that are included as the final focus of the realist portion of the review.
Initial Rough Theory: Controversies and Challenges Regarding Interventions
A realist review begins with an "initial crude theory," a beginning theory of what interventions are expected to exercise. Using this approach, the telescopic, focus, and refinement of the review evolve as the review gain; the procedure includes regular input from stakeholders.24 For this review, nosotros begin broadly, presenting the controversies and challenges in determining the reasons why diverse interventions or particular features of interventions may be constructive in irresolute HNHC patient health care apply.
Describing and Understanding Effective Interventions
In developing the protocol, we conferred with a Key Informant (KI) stakeholder panel to assistance ensure that the focus of the review would exist relevant to potential end users. The KI console consisted of ii clinician health researchers, one representative of a nongovernmental wellness policy organization and i representative from a health system research organization; 1 health system quality officeholder; and one statistician/survey scientist. (Section Ix describes the role of KIs.) KIs differed in their views virtually the nature of effective interventions for HNHC patients. Some thought that effective interventions could accept broad applicability and be relevant beyond multiple causes of high utilization. Others thought that constructive interventions need to be targeted to subpopulations of patients; what is effective for ane subpopulation may not be effective for another or only effective in certain circumstances and settings. The following are models of organizing the commitment of wellness care that are theorized equally the context for influencing and improving both intendance delivery and costs for HNHC patients.
Payer-Level Interventions
Accountable Care Organizations (ACOs). ACOs align financial incentives for care coordination and joint financial and health outcome accountability among a big grouping of wellness care providers across the health care continuum (ambulatory outpatient, acute care, mail service-astute care, and home health settings). An assumption underlying success in an ACO model is that providers, whether consciously or unconsciously, act to maximize the health of the patient while likewise maximizing their own financial incentive in caring for the patient. ACOs use a variety of strategies to achieve such goals, including the following:
- Increasing physicians' access to a uniform source of complete information well-nigh patients' health utilization and health condition to back up care coordination.
- Using techniques such as population segmentation and adventure stratification to focus resources on HNHC populations.
- Using diverse approaches to increasing coordination among health care settings, especially during transitions between settings in episodes of care:
- outpatient → ED → outpatient
- outpatient → inpatient → post-astute care → dwelling house wellness→ outpatient
Likewise, increasingly, ACOs include strategies to address social determinants of health. These strategies support the notion that addressing barriers to accessing appropriate wellness care services is as important as analogous care and ensuring equal access to care.
Patient-Centered Medical Homes (PCMH). The PCMH model encompasses five core attributes: comprehensive intendance, patient-centered care, coordinated intendance, attainable services, and quality/safety. Although this model is intended to promote changes in cost, access, and quality for all patients, it may take the greatest affect on HNHC patients because HNHC patients can yield the greatest reduction in expenditures and improvement in wellness outcomes. Care coordination is a central component, particularly during wellness care setting transitions (equally described in a higher place in relation to ACOs), based on the supposition that PCMHs tin can reduce unnecessary duplication of services and lower preventable utilization of wellness care in costly settings (predominately ED and inpatient care).
The implementation of PCMH models is broadly variable, simply most PCMHs encompass the five cadre attributes. The interaction of these five attributes may trigger the mechanisms that produce benign impact on health care expenditures and wellness outcomes of the HNHC population.
Home-Based Chief Care. Domicile-based primary intendance moves the delivery of the majority of master care from an ambulatory office-based setting to a patient's place of residence.25 Intended to be a comprehensive care commitment model, this model typically involves a team-based arroyo and combines home-based care for medical needs with intensive direction and care coordination. Dwelling house-based programs typically serve a population that has a high probability of being HNHC because participants commonly take complex chronic atmospheric condition and functional limitations. Habitation-based chief care may do good HNHC patients if such approaches can better accost patients' specific needs, values, and preferences. If HNHC patients take difficulty accessing traditional part-based care, home-based main intendance may exist peculiarly beneficial.
Clinicians are believed to be able to obtain greater insight into patient needs with home visits, frequently finding environmental and nonmedical factors related to patients' issues. HNHC patients may require frequent monitoring, intense direction, or rapid follow-up that cannot be easily accommodated by an function-based provider. Home-based chief care may too exist able to aid HNHC patients avoid complications from hospital care (due east.g., certain infections, delirium) when hospitalizations themselves can be averted or shortened. Several additional assumptions underlying the success of this arroyo is that the HNHC patients tin can exist identified, that intervening at abode is cost-effective, and that the teams work well together.
Health System and Provider-Level Interventions
At the wellness organization and clinician levels, data can be used to report health care service use that may betoken that a patient is HNHC and needs additional services. ED alerts inform clinicians that a patient has received care in the ED, which tin assist them identify patients whose patterns of care might be considered HNHC and in demand of additional support services. Hotspotting uses data to identify patients whose costs are outliers, such as the HNHC population; sympathize the problem; dedicate resources; and design effective interventions.26 Hotspotting typically includes multidisciplinary, coordinated care that treats the whole patient and attends to the nonmedical and social determinants that bear on health, including housing, mental wellness, substance abuse, and emotional back up. The underlying premise is that intensive and highly individualized care, addressing the unique needs of an HNHC patient, including social determinants of health, will amend health outcomes and reduce health expenditures beyond the cost of the high intensity, highly individualized hotspotting intervention.
Wellness-Related Interventions
At the patient level, supportive services and social determinants of wellness-related interventions can affect the success or failure of complex social interventions. They are intended to bridge the gap betwixt wellness care professionals who evangelize straight care and an individual patient. Persons in a variety of roles may provide supportive services, such every bit social workers, community health workers, patient navigators, and peer-to-peer networks.
Patient support services are intended to address mutual barriers related to resource limitations, education, and treatment adherence, thereby improving patient outcomes. Relatedly, the environment and social determinants of health, such as depression income, poor educational activity and nutrition, homelessness, and lack of transportation, have been identified equally predisposing factors limiting admission to care. For example, stable housing could improve patients' power to collaborate consistently with their health intendance providers and social back up systems, which, in turn, could increment adherence to their treatment plan.27
Applying a Clear Classification Taxonomy
A challenge in conducting a review on management of HNHC patients is the absence of a consensus in the field of a unifying classification schema or taxonomy of interventions. This gap complicates organizing key dimensions of these interventions into meaningful distinctions for grouping and separating their components.28
Intervention classification in recent systematic reviews regarding HNHC patients differs significantly. 1 systematic review stratified interventions as dwelling house-based, clinic-based, and principal intendance augmentation.15 Some other categorized interventions into case management, private care plans, and information sharing.13 Baker and colleagues stratified interventions by population type: adults (i) with two or more chronic diseases, (2) with i chronic affliction and low, and (iii) identified equally at take chances for loftier health care utilization.14
We advise to organize our findings starting with a taxonomy of interventions that maps to mechanisms that the review squad theorizes are related to the success of interventions for HNHC patients. We will effort to separately accost context, outcomes, and mechanisms at the payer, health care system, provider, and patient levels and those that cut beyond interventions.
II. The Key Questions
Cardinal Questions Initially proposed Key Questions (KQs) were posted for public annotate February 7, 2019, through March vii, 2019. We received comments from two individuals. The first individual wrote, "As important as identifying high utilization/high cost patients is understanding patterns of persistence from year to yr. That is critical for prioritization of interventions and the most effective interventions for patients with one or ii years of high toll versus multiple ongoing years." We agree with the comment. In describing HNHC patients (KQ 1), nosotros will limit the population to individuals with at least one year of high-price intendance. Within that population, we will present the patterns of persistent health care employ and costs described in the studies. The second private commented that being breastfed is a "stiff heath indicator" and would similar the review to include the relationship between having been breastfed every bit a child and being HNHC equally an adult. While this may be a salient characteristic of the HNHC population, for this assay, we need to exist able to observe past or predicted high utilization. Nosotros did not detect whatsoever studies that examine the human relationship between breastfeeding in infancy with high utilization in adulthood.
Tabular array 1 outlines the noun changes between the preliminary KQs and those included in this protocol. The "final" KQs appear below the table.
Tabular array one. Changes to KQs and PICOTS
| Original Element | Source | Comment | Decision and Changes | Rationale (Implications for Prove Report) |
|---|---|---|---|---|
| Population name | KI | KIs idea the term "high utilizer" should be changed to "high- need, loftier-cost (HNHC)," which has get a more ordinarily used term. | Change made | No implications for the workload of the review |
| KQ 1 | EPC | The EPC modified KQ i. KQ 1a-KQ 1e accept not been modified. | Original question: What are the characteristics of patients who are "high utilizers"? Protocol revised question: (see beneath) | The EPC modified KQ 1 for clarity. |
| KQ ii | EPC | The EPC modified KQ 2 to follow the format of a realist review. | Original question: What are the constructive interventions for adults identified as high utilizers of wellness care? Protocol revised question: (see below) | The EPC modified KQ 2 to reply this question using a realist review approach. The edits are intended to back up the goal of agreement the mechanisms that explicate successful outcomes in complex interventions serving HNHC patients. |
| KQ 3 | EPC | The EPC intends to answer KQ 3, using systematic review methods to support the findings concerning the interventions included in answering KQ 2, using realist review methods. | Original question: Overall, what is the show about which interventions targeting which patient groups lead to the highest overall improvement in health outcomes and cost savings for patients, clinicians, providers, and payers? Protocol revised question: (see below) | The original question was a comparative effectiveness question. Based on our conversations with KIs and our initial review of the literature, we believe that it will exist valuable to the field to focus on the more fundamental question of why and how particular interventions work (KQ 2) and the evidence of effectiveness and harms of these interventions (KQ three). |
EPC = Prove-based Practice Center; HNHC = high-need, high-cost; KI = Key Informant; KQ = Key Question.
- KQ i ("all-time fit" framework synthesis): What criteria identify or can be used to predict that patients volition be HNHC and why?
- KQ 1a. How do criteria incorporate patient clinical characteristics?
- KQ 1b. How do criteria incorporate patient health behaviors and sociodemographic characteristics (eastward.g., age, social determinants of health, insurance status and source of coverage, and access to the health care system)?
- KQ 1c. How do criteria contain types, corporeality, duration, and patterns of persistent apply of potentially preventable or modifiable health intendance use?
- KQ 1d. Do criteria differ at the payer, health care system, or provider levels?
- KQ 1e. How can observed or predicted potentially preventable or modifiable high employ of health care be differentiated from necessary and appropriate apply?
- KQ 2 (realist review): What are the mechanisms that lead to reductions in potentially preventable or modifiable health care use and result in improved health outcomes and cost savings in interventions serving HNHC patients?
- KQ 2a. What are the of import contexts, such equally the characteristics of the HNHC patients, the broader health care delivery organisation, and the community, that impact whether mechanisms facilitate the desired outcomes?
- KQ 3 (systematic review): Overall, what is the effectiveness and harms of interventions, included in answering KQ ii, in reducing potentially preventable or modifiable health intendance employ and costs and improving health outcomes among HNHC patients?
PICOTS and Classification Taxonomy
We made no substantive changes to the population, interventions, comparators, outcomes, timing, settings, and report design (PICOTS). As we proceed with the review, we anticipate that we will further focus our analysis and want to discuss decisions with our Technical Skillful Console (TEP) on multiple occasions. These occasions can include whatsoever or all of the following:
- Receiving input on whether we take identified the relevant studies or programs and, if we take not, where to notice additional information.
- Refining the HNHC population for the purposes of the review, including whether to combine subpopulations or continue them separate.
- Discussing the theories of why and when diverse mechanisms are activated by constructive complex interventions within particular contexts to produce outcomes.
Our final goal is to nowadays our findings within the context of a unifying classification schema or taxonomy. We may seek feedback from our TEP and members of our KI stakeholder console on whether what we develop will be useful to individuals and organizations that are seeking actionable information.
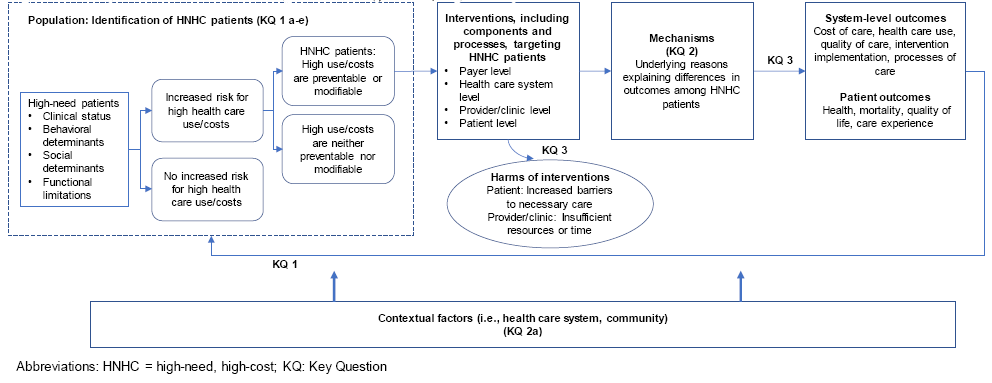
Iii. Analytic Framework
Figure 1 presents the analytic framework for the review and depicts the KQs in relation to the PICOTS. The figure illustrates how HNHC patients may be identified, how interventions that target HNHC patients together with contextual factors trigger different mechanisms of action that may result in systems-level outcomes (i.e., price, utilization, and quality of intendance) and patient outcomes (i.e., wellness, mortality, and patient experience), and harms that may occur because of the interventions.
Figure ane. Analytic framework for direction of loftier-need, loftier-toll patients
IV. Methods
Criteria for Inclusion/Exclusion of Studies in the Review
Table 2 presents the initial inclusion and exclusion criteria for the PICOTS of the review. In keeping with realist review methods, we will refine the scope of the review as we uncover testify and focus the depth and latitude of the review.29 We will address KQ 1 using a "best fit" framework synthesis methodology and KQ 2 using a realist review methodology; with these approaches, all written report designs, if relevant, are admissible for inclusion. We will answer KQ 3 using a systematic review methodology, resulting in admissible written report designs being more express.
Table ii. Inclusion/exclusion tabular array
| PICOTS | Inclusion | Exclusion |
|---|---|---|
| Population | KQs 1, ii, and 3: Noninstitutionalized adults, 18 years of age or older. KQ 1: Ane or more years of potentially preventable or modifiable high health intendance cost and/or utilise. KQs 2 and iii, 2 groups: | Patients receiving a high level of health care services that are considered appropriate for their condition OR high level of wellness care services are measured for less than 1 year OR end-of-life intendance |
| Intervention | KQ one: Not relevant, interventions not necessary for inclusion. KQs 2 and three: | KQs 2 and 3: Interventions for which the relevance for and impact on HNHC patients cannot exist adamant. |
| Comparator | KQ 1: Comparing population or no comparator KQ 2: Any intervention, handling as usual, or no comparator intervention. | KQ 3: No comparator |
| Outcomes | KQ i: Population characteristics described or predicted. KQs i, 2, and 3: | All other outcomes, including behavioral health outcomes |
| Time frame | Potentially preventable or modifiable high cost health care utilise measured for 1 year or more than. KQ iii: Measurement of outcomes at 1 year or more after implementation of the intervention. | Shorter time periods |
| Settings | Health care and support services delivery settings, including outpatient, ED, the broader wellness intendance delivery environment, customs characteristics related to social determinants of health. KQ 1: United States. KQs 2 and 3: patient-level interventions: very loftier homo development index countries; Health arrangement or payer-level interventions: United States. | Institutional intendance settings, such as hospitals, skilled nursing, long-term intendance facilities, and prisons or jails |
| Study design | KQs 1 and two: All study designs except reviews summarizing across original studies or interventions. KQ 3: Randomized controlled trials, cluster randomized trials, accomplice studies, case-control studies, quasi-experimental designs with a comparison group. | KQ three: All other designs |
| Linguistic communication | Studies published in English | Studies published in languages other than English |
| Publication Type | All publications that allow abstraction and interpretation of findings | KQ 3 only: Abstruse-but publications |
ACO = Answerable Care Organization; ED = emergency department; Ems = emergency management services; HNHC = high-need high-cost; KQ = Primal Question; PICOTS = population, intervention, comparator, outcomes, time frame, settings
Searching for the Bear witness: Literature Search Strategies to Identify Relevant Studies to Answer the Cardinal Questions
Areas of Focus for Searches
We will carry this review following the methodology of a "best fit" framework synthesis (for KQ i), realist review (for KQ two), and a systematic review (for KQ 3).22 In conducting the realist review, nosotros anticipate that starting from our rough theory, our searches will be iterative in a fashion that will enable u.s.a. to uncover the underlying mechanisms in circuitous interventions that are related to approaches or components that may exist effective with HNHC patients in unlike contexts and why.
To respond KQ 1, our goal is to review the evidence to develop an actionable description of HNHC patients that captures the distinguishing characteristics of populations whose high utilization is potentially modifiable. Based on input from our KI stakeholders during development of the protocol, HNHC populations volition be identified in our searches through unlike approaches, including the following:
- Multiple health conditions (i.eastward., multiple co-occurring chronic conditions, including behavioral health conditions).
- Multiple health atmospheric condition coupled with boosted risk factors (i.e., functional limitations, behavioral factors, financial factors, or social risk factors).
- Health services utilize (e.g., overuse of ED, inpatient, or other high-cost services).
To answer KQs two and 3, our attention volition focus on the following kinds of interventions:
- Complex structural changes and alternative financial arrangements (e.chiliad., ACOs, PCMHs, and health homes).
- Novel approaches to delivering services and providing information to clinicians (e.g., interdisciplinary teams, hotspotting).
- Calculation whatever patient-centered component to an existing wellness care commitment system (e.k., patient navigator, peer back up, and caregiver supports).
Nosotros also expect relevant interventions to be a source for further defining populations of involvement.
Sources of Literature
To begin to identify articles relevant to the review, nosotros initially conducted a focused search of MEDLINE via PubMed search (Appendix A). Our broader search will include both databases and gray literature sites, including Cochrane Clinical Trials Central Register, PsycINFO, Cumulative Index of Nursing and Allied Health Literature, EMBASE, Web of Science, Clinicaltrials.gov, and Academic Search Premier.
Our overall search results fall into three "buckets" because we will demand to use more than one approach to finding the literature that identifies HNHC patient populations and, relatedly, relevant interventions. The buckets are as follows:
- Studies identifying the population by using the text terms "high utilizer/medically complex/high needs" and like terms. Medical Subject Heading (MeSH) terms are not bachelor to identify the population using these types of terms.
- Studies identifying the population past using the MeSH term "multiple chronic conditions" or like terms, limited to individuals with functional limitations, behavioral factors (eastward.grand., wellness hazard behaviors or serious mental affliction), or social risk factors.
- Studies identifying populations by limiting them to specific weather or combinations of conditions (e.thou., cardiovascular affliction, diabetes, or both), when such populations likewise had functional limitations or behavioral or social risk factors.
Nosotros will also search for evaluation reports or other gray literature on government websites. These volition include the following: the Centers for Medicare & Medicaid Services, particularly its Center for Medicare and Medicaid Innovation, which supports development of Medicaid demonstrations and other alternative payment models; the National Plant on Drug Abuse; the Centers for Disease Control and Prevention; the National Constitute on Aging; the Human Resources Services Administration; the Veterans Administration; the National Library of Medicine (for HSRProj), and Social Work Abstracts. Nongovernment-sponsored studies will exist searched on websites of such organizations as the Camden Coalition, the Center for Health Care Strategies, the Republic Fund, the Kaiser Family Foundation, the Milbank Memorial Fund, the National Academy of Medicine, Patient-Centered Outcomes Inquiry Plant, the Robert Wood Johnson Foundation, and the Social Interventions Research & Evaluation Network Bear witness Library.
Following our preliminary searches as recommended for a realist review, nosotros will conduct snowball searches, including reviewing reference lists of included studies, identifying whether included studies are cited in newer articles, and looking for related studies, such as those suggested past PubMed.30 In addition, we know that we will need to relax our population restrictions to examine whether some studies of interventions, such as those related to ACOs, health homes, customs health workers, patient navigators, care managers, and others, focus on patients who are at risk of being HNHC and thus may not be identified through i of our three population buckets.
Quality Assurance for Searches
Nosotros will conduct quality checks to ensure our search identifies known studies. If not, we will revise and rerun our searches. An experienced librarian familiar with systematic reviews will design and acquit all searches in consultation with the review squad. Nosotros volition also behave an updated literature search (of the same databases searched initially) concurrent with the process for peer and public review of the draft report. We will investigate whatever literature that peer reviewers or the public suggest and, if advisable, volition incorporate them into the concluding review. We will identify all eligible studies using the same criteria described above.
Information Abstraction and Data Management
As with systematic reviews, a broad range of documents can exist relevant in a realist synthesis. Two trained inquiry team members will independently review all titles and abstracts identified through searches for eligibility against our inclusion/exclusion criteria using Abstrackr.31 Studies marked for possible inclusion by either reviewer will undergo a full-text review. For studies without adequate information to determine inclusion or exclusion, we will retrieve the total text and so brand the determination. All results volition be tracked in an EndNote® bibliographic database (Thomson Reuters, New York, NY).
We will recall and review the full text of all titles included during the title/abstruse review stage and through hand searches. Two trained team members will independently review each full-text commodity for inclusion or exclusion based on the eligibility criteria described above (Tabular array 3). If both reviewers agree that a study does not see the eligibility criteria, the study will be excluded. If the reviewers disagree, conflicts volition be resolved by discussion and consensus or by consulting a tertiary member of the review team. As described to a higher place, all results will be tracked in an EndNote database.
For the realist review, we volition evaluate manufactures for their relevance and robustness in answering the review questions and their contribution to theory building and testing. For all KQs, nosotros will also evaluate articles as to whether the methods that authors used to generate data are credible and trustworthy.29 Nosotros volition record the reason that we concluded that whatever excluded full text did non satisfy the eligibility criteria and so that we can later on compile a comprehensive list of such studies.
For studies that come across our inclusion criteria, we volition abstract relevant information into tables. To answer the realist review question (KQ two), we volition abstract data relevant for our analyses and synthesis, including context, intervention, mechanisms, outcomes, and theories. We expect to refine the data extraction process continually as the review progresses; nosotros anticipate information selection and appraisal will be ongoing and conducted in parallel with the analysis.29
To reply the systematic review question (KQ three), we will design evidence tables to get together pertinent information from each commodity; these data will include characteristics of study populations, settings, interventions, comparators, study designs, methods, and results. Trained reviewers will extract the relevant data from each included commodity into the evidence tables. A 2nd member of the team will review all information abstractions for completeness and accuracy.
Realist Review: Quality Appraisal
Quality appraisement in realistic reviews is not focused on assessing the risk of bias of individual studies simply rather on assessing the rigor used to develop one or more than program theories. In realist reviews, assessing study rigor occurs throughout the procedure of synthesis and includes all of the key aspects of the review process: the quality of the theory evolution, the data identified equally relevant and analyzed, and the inferences made from the data.32
We will, therefore, appraise data based on relevance (whether included manufactures tin contribute to theory building and testing), trustworthiness (whether the information in a study have been obtained empirically, using methods that are clearly stated and whether the data could exist establish in more than one source), plausibility of the argument underlying the theory (the coherence of the argument, including its breadth in explaining the data, its simplicity and fit with existing theory), and rigor (whether included articles are methodologically apparent with regard to outcomes reported and methods used for testing propositions). Our appraisal approach will consider how our findings (theory and observation of relationships) have evolved at each evidential footstep. As such, we will use RAMESES project standards to guide our judgments in quality appraisement tasks.29,32-34
Previous realist reviews have applied qualitative methods to appraisal. Standards tools include the UK Cabinet Role quality framework and a Critical Appraisal Skills Programme tool.34 Even so, according to a study comparing appraisal methods in realist reviews, Dixon-Woods et al.35 constitute tool-based approaches to be similar in the level of agreement to those using unprompted judgment.
Assessment of Methodological Quality or Risk of Bias of Individual Studies
For KQs 1 and 2, nosotros volition appraise each included qualitative enquiry study in terms of rigor and validity using the Critical Appraisement Skills Programme checklist for qualitative research.38 Our goal is to take a consistent arroyo for evaluating the strengths and limitations in private studies. All the same, as recommended past the authors of the checklist, the results volition not be used to create a scoring arrangement. Descriptive studies that count or seek to place characteristics of HNHC patients will be assessed in relation to the threat of option bias and misreckoning, as relevant. Other studies, such as theory and opinion used to respond KQ 2, will be solely appraised using the realist review quality appraisal approach discussed above.
For KQ 3, we volition use the criteria set forth by the Bureau for Healthcare Quality and Research's (AHRQ's) Methods Guide for Comparative Effectiveness Reviews. To assess the risk of bias (i.due east., internal validity), we volition use the ROBINS-ane39 tool for observational studies and the Cochrane randomized controlled trial (RCT) toolforty for RCTs. For both RCTs and observational studies, risk of bias cess will include questions to assess all the following:
- Various types of bias, including selection bias, confounding, performance bias, detection bias, and attrition bias.
- Concepts about adequacy of randomization (for RCTs but), such as similarity of groups at baseline, and masking.
- Method of handling dropouts and missing information, whether intention-to-treat analysis was used, reliability and validity of outcome measures, and treatment fidelity.41
Two independent reviewers will assign adventure of bias ratings for outcomes from each report; they volition also specify when the risk of bias for an individual outcome may be lower than the rating for the report overall. Disagreements between the two reviewers will exist resolved by discussion and consensus or by consulting a 3rd member of the team.
We volition requite a low risk of bias rating for outcomes that meet all criteria. Studies that exercise not report their methods sufficiently may be rated every bit unclear take chances of bias. We will give a high risk of bias rating to outcomes from studies that take a methodological shortcoming in i or more categories and will exclude them from our main analyses.
Data Synthesis
Realist Review: 3 Main Targets of Analysis
In a realist review, the goal of the synthesis is to develop and then "test" (ostend, refute, or refine), confronting the information from included documents, realist causal explanations for outcomes. Analysis of the data should as well be directed to understanding the relationships of the CMO configurations that have been developed inside the program theory or theories. The realist causal caption for outcomes takes the class of CMO configurations. Specifically, a CMO configuration describes and explains the relationship between particular features that have been interpreted as functioning as context, particular mechanisms, and particular outcomes. In a judgement, such a CMO presentation will take the form of "In 'X' context, 'Y' mechanism is activated or triggered, and it causes 'Z' upshot." The synthesis presents evidence to support two chief conclusions: (1) that the specific features of context exist and affect the activation of a mechanism of action (entities, processes, or structures) and (2) that the hypothesized mechanisms exist and cause outcomes.24
Systematic Review: Procedures for Analysis and Synthesis
For KQ 3, we will follow standard EPC (AHRQ) procedures to summarize all included studies in narrative grade and in summary tables that tabulate the of import features of the written report populations, design, intervention, outcomes, setting (including geographic location), and results. Autonomously from documenting basic study characteristics, nosotros will include findings but from studies of low, medium, or unclear adventure of bias in our main written report, which nosotros will synthesize either qualitatively or quantitatively (insofar equally possible).
Findings from studies determined to be of high risk of bias will appear in the evidence tables in the appendix. If feasible, we may exercise qualitative or quantitative sensitivity analyses to estimate the departure in conclusions stemming from including and excluding studies considered high take a chance of bias.
If we find 3 or more than studies for a comparison of an upshot of interest, nosotros will consider pooling our findings past using quantitative analysis (i.east., meta-assay) of the information from those studies. We will as well consider conducting network meta-analysis using Bayesian methods to compare the interventions with each other if nosotros place at to the lowest degree three studies that tested the same intervention with a common comparator. For all analyses, we will apply random effects models to estimate pooled or comparative effects; dissimilar a fixed-effects model, this approach allows for the likelihood that the true population effect may vary from study to study. To make up one's mind whether quantitative analyses are appropriate, nosotros will appraise the clinical and methodological heterogeneity of the studies under consideration following established guidance.
Systematic Review: Grading the Strength of Testify
For KQ iii, nosotros will form the strength of evidence (SOE) based on the guidance established for the EPC Plan.42 Developed to class the overall strength of a trunk of evidence, this approach incorporates five cardinal domains: risk of bias (includes study design and aggregate quality), consistency, directness, precision of the evidence, and reporting bias. It also considers other optional domains that may be relevant for some scenarios, such as a dose-response clan, plausible confounding that would decrease the observed outcome, and strength of association (magnitude of upshot).
Table three describes the grades of evidence that tin exist assigned. Grades reverberate the strength of the body of prove to answer KQs on the effectiveness and harms of the interventions included in this review. Two reviewers will appraise each domain for each cardinal outcome; they will resolve any differences past consensus word. If the volume of evidence is big, we may focus the SOE grading on outcomes of substantial importance to decisionmakers and those commonly reported in the literature.
Tabular array three. Definitions of the grades of overall strength of bear witness42
| Grade | Definition |
|---|---|
| High | High confidence that the evidence reflects the true consequence. Further research is very unlikely to change our confidence in the gauge of effect. |
| Moderate | Moderate confidence that the evidence reflects the truthful consequence. Further research may modify our confidence in the estimate of the effect and may change the estimate. |
| Low | Low confidence that the evidence reflects the truthful effect. Further inquiry is probable to modify our conviction in the gauge of the effect and is probable to modify the estimate. |
| Insufficient | Evidence either is unavailable or does not permit interpretation of an outcome. |
Assessing Applicability
We volition assess the applicability of individual studies equally well equally the applicability of a trunk of evidence following guidance from the Methods Guide for Effectiveness and Comparative Effectiveness Reviews.43 We expect to be able to practice this for all three KQs.
For individual studies, we will examine weather that may limit applicability based on the PICOTS structure. The cess of applicability is integral to a realist review through its consideration of context within CMO configurations. Nosotros volition nowadays when patterns across studies either were not tested or do non announced to operate similarly in particular settings.
V. References
1. Centers for Medicare & Medicaid Services. CMS proposes "pathways to success," an overhaul of Medicare's ACO program. Baltimore, MD: Centers for Medicare & Medicaid Service; 2018. https://www.cms.gov/newsroom/printing-releases/cms-proposes-pathways-success-overhaul-medicares-aco-plan?_ga=2.111400452.1093732935.1551231053-96630637.1551231053. Accessed on February 27,, 2018.
2. Centers for Medicare & Medicaid Services. Medicare-Medicaid accountable intendance organization (ACO) model. Baltimore, Doctor: Centers for Medicare & Medicaid Services; 2016. https://www.cms.gov/newsroom/fact-sheets/medicare-medicaid-accountable-intendance-organization-aco-model. Accessed on February 27,, 2019.
3. Centers for Medicare & Medicaid Services. Vermont all-payer ACO model. Baltimore, MD: Centers for Medicare & Medicaid Services; 2016. https://www.cms.gov/newsroom/fact-sheets/vermont-all-payer-aco-model. Accessed on February 27,, 2019.
iv. Centers for Medicare & Medicaid Services. CMS finalizes "pathways to success," an overhaul of Medicare's national ACO program. Baltimore, MD: Centers for Medicare & Medicaid Services; 2018. https://www.cms.gov/newsroom/printing-releases/cms-finalizes-pathways-success-overhaul-medicares-national-aco-program. Accessed on February 27,, 2019.
5. Brennan A, Gaus C. ACOs at a crossroads: costs, risk and MACRA. A NAACOS policy white newspaper. Washington, DC: National Association of ACOs,; 2016. https://world wide web.naacos.com/acos-at-a-crossroads Accessed on Feb 27,, 2019.
6. Hagland M. NAACOS and ACO leaders express distress over just-announced MSSP application deadline. Sarasota, FL: Healthcare Innovation; 2019. https://www.hcinnovationgroup.com/population-wellness-management/article/13031036/naacos-and-aco-leaders-express-distress-over-justannounced-mssp-application-borderline. Accessed on February 27,, 2019.
7. Cohen S. The concentration of wellness care expenditures and related expenses for costly medical conditions, 2012. Statistical Brief #455. Rockville, Dr.: Agency for Healthcare Inquiry and Quality; 2014. http://www.meps.ahrq.gov/mepsweb/data_files/publications/st455/stat455.pdf.
8. Cohen SB. The concentration and persistence in the level of health expenditures over time: estimates for the U.Due south. population, 2011–2012. Statistical Brief #449. Rockville, MD: Agency for Healthcare Research and Quality; September 2014. http://world wide web.meps.ahrq.gov/mepsweb/data_files/publications/st449/stat449.shtml.
ix. Cohen SB. The concentration of health intendance expenditures in the U.Due south. and predictions of future spending. J Econ Soc Meas. 2016;41:167–89.
10. Centers for Medicare & Medicaid Services. Medicare beneficiaries at a glance. Baltimore, Physician: Centers for Medicare & Medicaid Services; 2019. https://www.cms.gov/Research-Statistics-Information-and-Systems/Statistics-Trends-and-Reports/Beneficiary-Snapshot/Bene_Snapshot.html. Accessed on February 27,, 2019.
11. Centers for Medicare & Medicaid Services. All Medicare inpatient hospitals: utilization, program payments, and cost sharing for original medicare beneficiaries, by demographic characteristics and Medicare-Medicaid enrollment status, calendar yr 2017. Baltimore, Md: Centers for Medicare & Medicaid Services; north.d. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/CMSProgramStatistics/2017/Downloads/UTIL/2017_CPS_MDCR_INPT_HOSP_2.PDF. Accessed on February 27,, 2019.
12. Moe J, Kirkland SW, Rawe E, et al. Effectiveness of interventions to decrease emergency department visits by adult frequent users: a systematic review. Acad Emerg Med. 2017 Jan;24(1):xl-52. doi: 10.1111/acem.13060. PMID: 27473387.
13. Soril LJ, Leggett LE, Lorenzetti DL, et al. Reducing frequent visits to the emergency department: a systematic review of interventions. PLoS 1. 2015;10(iv):e0123660. doi: 10.1371/journal.pone.0123660. PMID: 25874866.
14. Bakery JM, Grant RW, Gopalan A. A systematic review of care management interventions targeting multimorbidity and high intendance utilization. BMC Health Serv Res. 2018 Jan xxx;18(i):65. doi: 10.1186/s12913-018-2881-eight. PMID: 29382327.
15. Edwards ST, Peterson K, Chan B, et al. Effectiveness of intensive primary intendance interventions: a systematic review. J Gen Intern Med. 2017 Dec;32(12):1377-86. doi: 10.1007/s11606-017-4174-z. PMID: 28924747.
16. Smith SM, Wallace E, O'Dowd T, et al. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2016 Mar 14;3:CD006560. doi: 10.1002/14651858.CD006560.pub3. PMID: 26976529.
17. Cohen S, Yu W. The concentration and persistence in the level of health expenditures over time: estimates for the U.S. population, 2008–2009. Statistical Cursory #354. Rockville, MD: Agency for Healthcare Research and Quality; Jan 2012. http://www.meps.ahrq.gov/mepsweb/data_files/publications/st354/stat354.pdf.
xviii. Pearson SD, Katzelnick DJ, Simon GE, et al. Depression among high utilizers of medical care. J Gen Intern Med. 1999;14(viii):461-eight. doi: ten.1046/j.1525-1497.1999.06278.ten.
19. Katon W, Von Korff M, Lin E, et al. Distressed high utilizers of medical care. DSM-Three-R diagnoses and treatment needs. Gen Hosp Psychiatry. 1990;12(6):355‐62. PMID: CN-00071507.
xx. National Academy of Medicine. Effective care for high-demand patients. Opportunities for improving outcomes, value, and health. Washington, DC: National University of Sciences; 2017.
21. Carroll C, Booth A, Leaviss J, et al. "Best fit" framework synthesis: refining the method. BMC Med Res Methodol. 2013 Mar xiii;13:37. doi: x.1186/1471-2288-xiii-37. PMID: 23497061.
22. Pawson R, Greenhalgh T, Harvey G, et al. Realist review--a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy. 2005 Jul;10(Suppl 1):21-34. doi: x.1258/1355819054308530. PMID: 16053581.
23. Greenhalgh T, Wong Chiliad, Westhorp G, et al. Protocol--realist and meta-narrative evidence synthesis: evolving standards (RAMESES). BMC Med Res Methodol. 2011;xi:115-. doi: x.1186/1471-2288-eleven-115. PMID: 21843376.
24. Wong Grand, Westhorp G, Pawson R, et al. Realist synthesis RAMESES training materials London: National Found for Health Enquiry Health Services and Delivery Enquiry Programme; July 2013.
25. Totten A, White-Chu E, Wasson N, et al. Home-based master care interventions. Comparative Effectiveness Review No. 164. (Prepared by the Pacific Northwest Evidence-based Practise Heart under Contract No. 290-2012-00014-I.). AHRQ Publication No. xv(xvi)-EHC036-EF. Rockville, Dr.: Agency for Healthcare Research and Quality; February 2016.
26. Association of American Medical Colleges. Hot spotting guide FAQ. Washington, DC: Association of American Medical Colleges; 2019. https://www.aamc.org/initiatives/hotspotter/faqs/372468/hotspottingguidefaq.html. Accessed on August 12, 2019.
27. National Clan of Customs Health Centers. Health care for the homeless. Bethesda, MD: National Association of Community Health Centers, Inc.; 2019. http://www.nachc.org/health-center-issues/special-populations/health-care-for-the-homeless/. Accessed on August 12, 2019.
28. Guise JM, Chang C, Butler M, et al. AHRQ series on complex intervention systematic reviews-paper 1: an introduction to a series of articles that provide guidance and tools for reviews of circuitous interventions. J Clin Epidemiol. 2017 October;90:6-10. doi: ten.1016/j.jclinepi.2017.06.011. PMID: 28720511.
29. RAMESES Project. Quality standards for realist synthesis (for researchers and peer-reviewers). Oxford: Nuffield Section of Primary Care Wellness Sciences, Academy of Oxford; 2014. www.ramesesproject.org). Accessed on August 12, 2019.
30. Wong Chiliad, Greenhalgh T, Westhorp Yard, et al. Evolution of methodological guidance, publication standards and grooming materials for realist and meta-narrative reviews: the RAMESES (Realist and Meta-narrative Evidence Synthesis - Evolving Standards) project. Health Services and Delivery Inquiry 2014;2 doi: x.3310/hsdr02300.
31. Wallace BC, Small K, Brodley CE, et al. Deploying an interactive car learning system in an evidence-based do heart: Abstrackr. Proc. of the ACM International Health Informatics Symposium (IHI); 2012. 1038: pp. 819-24.
32. Wong G. Data gathering for realist reviews: Looking for needles in haystacks. In: Emmel N, Greenhalgh J, Manzano A, Monaghan M, Dalkin S, eds. Doing realist research. London: Sage; 2018.
33. Wong Thou, Greenhalgh T, Westhorp G, et al. RAMESES publication standards: realist syntheses. BMC Med. 2013 2013/01/29;eleven(1):21. doi: 10.1186/1741-7015-11-21.
34. Berg RC, Nanavati J. Realist review: current do and futurity prospects. J Res Pract. 2016;12(1).
35. Dixon-Wood M, Sutton A, Shaw R, et al. Appraising qualitative research for inclusion in systematic reviews: a quantitative and qualitative comparison of three methods. J Health Serv Res Policy. 2007 Jan;12(one):42-seven. doi: ten.1258/135581907779497486. PMID: 17244397.
36. Band North, Ritchie K, Mandava L, et al. A guide to synthesising qualitative research for researchers undertaking health technology assessments and systematic reviews. University of Stirling, School of Nursing, Midwifery and Health. Scotland: NHS Quality Improvement Scotland; 2011.
37. Barnett-Page Eastward, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol. 2009 Aug 11;9:59. doi: 10.1186/1471-2288-nine-59. PMID: 19671152.
38. Critical Appraisal Skills Programme. CASP qualitative checklist. [online]. Oxford: Critical Appraisal Skills Programme; 2018. https://casp-u.k..net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf. Accessed on November vii, 2019.
39. Sterne JA, Hernan MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016 Oct 12;355:i4919. doi: 10.1136/bmj.i4919. PMID: 27733354.
forty. Higgins JPT, Dark-green S. Cochrane handbook for systematic reviews of interventions. The Cochrane Collaboration; 2011. www.handbook.cochrane.org. Accessed on Jan 10, 2017.
41. Agency for Healthcare Research and Quality. Methods guide for effectiveness and comparative effectiveness reviews. AHRQ Publication No. 10(fourteen)-EHC063-EF. Rockville, Doc: Agency for Healthcare Research and Quality; Jan 2014. www.effectivehealthcare.ahrq.gov.
42. Berkman ND, Lohr KN, Ansari MT, et al. Grading the strength of a body of evidence when assessing health care interventions: an EPC update. J Clin Epidemiol. 2015 Nov;68(11):1312-24. doi: 10.1016/j.jclinepi.2014.xi.023. PMID: 25721570.
43. Atkins D, Chang SM, Gartlehner Thou, et al. Assessing applicability when comparing medical interventions: AHRQ and the Constructive Health Intendance Program. J Clin Epidemiol. 2011 Nov;64(11):1198-207. doi: 10.1016/j.jclinepi.2010.11.021. PMID: 21463926.
Six. Definition of Terms
This section is not applicative.
Vii. Summary of Protocol Amendments
If we demand to amend this protocol, nosotros will give the date of each amendment, describe the change and give the rationale in this section. Changes will not be incorporated into the protocol. Table 4 below illustrates the arroyo.
Table 4. Tabular array of changes to protocol
| Date | Section | Original Protocol | Revised Protocol | Rationale |
|---|---|---|---|---|
| This should exist the constructive appointment of the modify in protocol | Specify where the alter would be institute in the protocol | Depict the language of the original protocol. | Describe the alter in protocol. | Justify why the modify will amend the report. If necessary, describe why the change does not innovate bias. Exercise non use justification every bit "because the AE/TOO/TEP/Peer reviewer told the states to" merely explain what the change hopes to accomplish. |
AE = acquaintance editor; TEP = Technical Expert Console; TOO = task society officer
VIII. Review of Key Questions
AHRQ posted the KQs on the AHRQ Constructive Wellness Care Website for public comment. The EPC refined and finalized the KQs after reviewing public comments and obtaining input from KIs and the TEP. This input is intended to ensure that the KQs are specific and relevant.
IX. Cardinal Informants
KIs are the end users of research. They can include patients and caregivers, practicing clinicians, relevant professional and consumer organizations, purchasers of health care, health intendance systems, payers, and others with experience in making health care decisions. Within the EPC program, the KI role is to provide advice about identifying the KQs for research that will inform health intendance decisions. The EPC solicits input from KIs when developing questions for systematic review or when identifying high-priority research gaps and needed new research.
KIs are non involved in analyzing the show or writing the written report; they as well have non reviewed the report, except as given the opportunity to exercise and so through the peer or public review machinery.
KIs must disclose any financial conflicts of interest greater than $5,000 and any other relevant business or professional person conflicts of interest. Considering of their role every bit end users, individuals are invited to serve every bit KIs and those who nowadays with potential conflicts may be retained. The AHRQ Task Order Officer (TOO) and the EPC work to residuum, manage, or mitigate any potential conflicts of involvement identified.
X. Technical Experts
Technical Experts establish a multidisciplinary group of clinical, content, and methodological experts who provide input in defining populations, interventions, comparisons, or outcomes and place studies or databases to search. They are selected to provide wide expertise and perspectives specific to the topic under development. Divergent and alien opinions are mutual and perceived as healthy scientific soapbox that results in a thoughtful, relevant systematic review. Therefore, study questions, pattern, and methodological approaches practise not necessarily represent the views of individual technical and content experts. Technical Experts provide information to the EPC to identify literature search strategies and suggest approaches to specific problems as requested by the EPC. Technical Experts do not practice analysis of whatsoever kind nor practice they contribute to the writing of the written report. They accept non reviewed the report, except as given the opportunity to do so through the peer or public review machinery.
Technical Experts must disembalm whatsoever financial conflicts of interest greater than $v,000 and any other relevant business or professional person conflicts of interest. Because of their unique clinical or content expertise, individuals are invited to serve as Technical Experts and those who nowadays with potential conflicts may exist retained. The AHRQ TOO and the EPC work to residuum, manage, or mitigate any potential conflicts of interest identified.
XI. Peer Reviewers
Peer Reviewers are invited to provide written comments on the draft report based on their clinical, content, or methodological expertise. The EPC considers all peer review comments on the draft report in preparing the final report. Peer Reviewers do not participate in writing or editing the final study or other products. The terminal report does not necessarily represent the views of individual reviewers. The EPC will complete a disposition of all peer review comments. The disposition of comments for systematic reviews and technical briefs will be published 3 months afterwards the publication of the bear witness report.
Potential Peer Reviewers must disembalm any fiscal conflicts of involvement greater than $five,000 and whatsoever other relevant business or professional conflicts of interest. Invited Peer Reviewers may non take any fiscal conflict of interest greater than $five,000. Peer Reviewers who disclose potential business concern or professional person conflicts of interest may submit comments on draft reports through the public annotate mechanism.
XII. EPC Team Disclosures
EPC core team members must disclose any financial conflicts of interest greater than $1,000 and whatever other relevant business or professional conflicts of involvement. Related financial conflicts of interest that cumulatively total greater than $1,000 will usually disqualify EPC core squad investigators.
13. Office of the Funder
This projection was funded under Contract No. HHSA290201500011I from AHRQ, U.Southward. Department of Health and Human Services. The AHRQ Also reviewed contract deliverables for adherence to contract requirements and quality. The authors of this report are responsible for its content. Statements in the report should not be construed as endorsement by AHRQ or the U.S. Department of Health and Human being Services.
Xiv. Registration
This protocol volition be registered in the international prospective register of systematic reviews (PROSPERO).
Appendix A
| Search | Query | Found |
|---|---|---|
| #1 | Search ((("high utilizer" OR "loftier utilizers of health care" OR "high utilizing" OR "super utilizers" OR "super utilizing" OR "frequent utilization" OR "frequent utilisation" OR "frequent utilizers" OR "heavy utilization" OR "heavy utilizers" OR "high attenders" OR "repeat users" OR "hyperusers" OR "revolving door patients" OR "hyperutilization" OR "overutilization" OR "recividism")) OR "frequent users") OR "frequent user" OR "medically circuitous" OR "high need" Sort by: Best Match | 3460 |
| #2 | Search ((("Multiple Chronic Conditions"[Mesh]) OR "Comorbidity"[Mesh]) OR "multimorbidity" [MeSH] Sort by: Best Lucifer | 100740 |
| #3 | Search ((((((((((((((((((("Diabetes Mellitus"[Mesh]) OR "Eye Failure"[Mesh]) OR "Cardiovascular Diseases"[Mesh]) OR "Hypertension"[Mesh]) OR "Pulmonary Disease, Chronic Obstructive"[Mesh]) OR "Asthma"[Mesh]) OR "Chronic Hurting"[Mesh]) OR "Headache"[Mesh]) OR "Anterior Wall Myocardial Infarction"[Mesh]) OR "Kidney Failure, Chronic"[Mesh]) OR "Dementia"[Mesh]) OR "Alzheimer Illness"[Mesh]) OR "Lung Diseases, Obstructive"[Mesh]) OR "Stroke"[Mesh]) OR "Arrhythmias, Cardiac"[Mesh]))) OR "chronic gastrointestinal disorder") OR "Coronary Illness"[Mesh] Sort past: Best Match | 3003277 |
| #4 | Search (("Disabled Persons"[Mesh]) OR "Delicate Elderly"[Mesh]) OR "Mobility Limitation"[Mesh] Sort past: Best Match | 75328 |
| #5 | Search (("health adventure behaviors") OR ("Behavioral Symptoms"[Mesh]) OR "Substance-Related Disorders"[Mesh]) OR "Depression"[Mesh]) OR "Anxiety"[Mesh]) OR "Cognitive Dysfunction"[Mesh])) OR (("serious mental illness") OR "chronic toxic stress") Sort by: Best Friction match | 654519 |
| #8 | Search ("Homeless Persons"[Mesh]) OR ((((((((("Social Determinants of Wellness"[Mesh]) OR "Social Isolation"[Mesh]) OR "Poverty"[Mesh]) OR "Educational Status"[Mesh]) OR "Literacy"[Mesh]) OR "Intimate Partner Violence"[Mesh]) OR "Medically Uninsured"[Mesh])) OR (((((("food insecurity") OR "housing instability") OR "unemployed") OR "physical rubber") OR "community deprivation") OR "adverse babyhood experiences")) Sort past: Best Friction match | 138695 |
| #ix | Search (#2 OR #iv OR #5 OR #8) Sort past: All-time Match | 918962 |
| #10 | Search (#3 AND #9) Sort past: Best Match | 105820 |
| #11 | Search (#3 AND #9) Sort by: Best Match Filters: Humans | 103615 |
| #12 | Search (#three AND #ix) Sort past: Best Match Filters: Humans; Developed: nineteen+ years | 75716 |
| #xiii | Search (#3 AND #ix) Sort by: Best Match Filters: Humans; English language; Adult: 19+ years | 67531 |
| #14 | Search (#3 AND #ix) Sort by: Best Match Filters: Publication engagement from 2000/01/01; Humans; English; Adult: 19+ years | 55068 |
| #sixteen | Search ((((((((((("Patient-Centered Intendance"[Mesh]) OR "Disease Management"[Mesh])) OR ((("health home") OR "Answerable Care Organizations"[Mesh]) OR "Managed Care Programs"[Mesh])) OR ("Community Wellness Workers"[Mesh]) OR "Example Management"[Mesh]) OR "intendance coordination") OR "patient intendance management")))) OR ((((((((((("hotspotting") OR "patient navigation"[MeSH Terms]) OR "care management") OR "multidisciplinary team care") OR "integrated behavioral health") OR "diversion strategies") OR "cocky management support") OR "health coaching") OR "transition care") OR "enhanced chief intendance") OR "interdisciplinary care")) OR "patient navigation")) OR ((((((((((("House Calls"[Mesh]) OR "Text Messaging"[Mesh] OR "dwelling house visit")) OR "pharmacy intendance management") OR "caregiver back up")) OR "medicaid management") OR "care management") OR "medication assist") OR "home care") OR "transitional care")) OR "warm handoff") OR "diversion team") Sort past: Best Lucifer | 207066 |
| #17 | Search (#14 AND #16) Sort by: Best Match | 1686 |
| #xviii | Search (#17 OR #one) Sort by: All-time Match | 5143 |
| #19 | Search (#17 OR #ane) Sort by: All-time Friction match Filters: English | 4987 |
| #20 | Search (#17 OR #1) Sort past: Best Lucifer Filters: English; Adult: 19+ years | 3229 |
| #21 | Search (#17 OR #ane) Sort by: Best Friction match Filters: Humans; English; Adult: 19+ years | 3229 |
| #22 | Search (#17 OR #1) Sort by: Best Lucifer Filters: Publication date from 2000/01/01; Humans; English; Adult: 19+ years | 3009 |
brainerdseestrocces.blogspot.com
Source: https://effectivehealthcare.ahrq.gov/products/high-utilizers-health-care/protocol
0 Response to "Medicare Behavioral Health Conflict of Interest Reporting and Review"
Post a Comment